 January 3rd was a bad day for Cee. That morning she had a colonoscopy. The procedure went smoothly. But afterward, Cee felt ill. Something wasn’t right. She had a bite to eat, poured a glass of milk, and told her husband she was going to lie down. She set the milk on her nightstand. Then she collapsed.
January 3rd was a bad day for Cee. That morning she had a colonoscopy. The procedure went smoothly. But afterward, Cee felt ill. Something wasn’t right. She had a bite to eat, poured a glass of milk, and told her husband she was going to lie down. She set the milk on her nightstand. Then she collapsed.
At the hospital, doctors determined Cee was having a stroke. They found a clot blocking a major artery in the left side of her brain, so they gave her a clot-busting drug called tPA and airlifted her to the stroke center at Swedish Medical Center in Denver. By the time she arrived at Swedish, the clot was gone — a good sign, the doctors said.
The left side of the brain controls the right side of the body. Cee was awake, but her entire right side was paralyzed. She couldn’t speak, nor was she responding to simple commands. But when she saw her husband and daughter, she smiled and started to cry.
Over the next couple of days, Cee improved. She said a few simple words, like “hi” and “light,” and she began moving her right leg. Her right arm, however, remained motionless. An MRI showed severe damage to left side of Cee’s brain, mainly the regions that control speech and language, but also the motor cortex. Her physician was not optimistic. He doubted she’d regain the use of her arm, or be able to return to work. Cee had been a go-getter in a fast-paced career. But now Cee would be lucky to function as a housewife, the doctor told her family.
I have been preoccupied with strokes and stroke recovery ever since January, when Cee, my 57-year-old aunt, collapsed 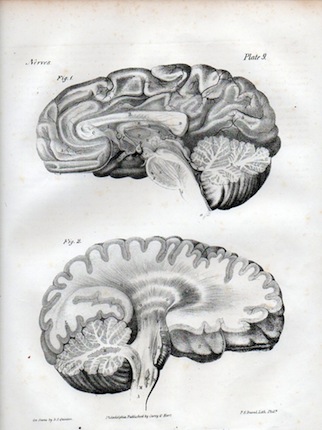 in her home in Colorado Springs. And, frankly, the grim prognosis her doctor offered royally pissed me off. Certainly recovery — even full recovery — after a stroke is possible. No one who has heard Jill Bolte Taylor’s amazing tale of re-learning how to talk, walk, and think after a blood vessel burst in her brain can doubt that. So why was my aunt’s doctor being such a pessimist? Was he simply trying to prepare us for the worst? Or, more frighteningly, did he actually see something in Cee’s MRI that made him certain she could not bounce back?
in her home in Colorado Springs. And, frankly, the grim prognosis her doctor offered royally pissed me off. Certainly recovery — even full recovery — after a stroke is possible. No one who has heard Jill Bolte Taylor’s amazing tale of re-learning how to talk, walk, and think after a blood vessel burst in her brain can doubt that. So why was my aunt’s doctor being such a pessimist? Was he simply trying to prepare us for the worst? Or, more frighteningly, did he actually see something in Cee’s MRI that made him certain she could not bounce back?
I wanted to find out how the brain recovers after a stroke, and what an MRI can and can’t say about a person’s ability to recover. So last weekend I tracked down neurologist Walter Koroshetz, deputy director of the National Institute of Neurological Disorders and Stroke, at the annual meeting of the American Association for the Advancement of Science in Washington, DC. (One of the perks of being a science writer is having access to top-tier scientists.)
During a normal stroke, a clot cuts off blood flow to part of the brain. (Blood vessels can also burst. But this type of stroke — called a hemorrhagic stroke — is less common.) The tissue deprived of oxygen-rich blood dies. “A hole gets created,” Koroshetz says. The neurons that used to reside in that region are gone. But other neurons can pick up the slack. Say you have a stroke victim like Cee who was left with a paralyzed arm. As that person recovers, he or she may regain the ability to move the arm. If you put that person in a functional MRI machine and ask him or her to move the once-paralyzed limb, large areas of the brain will light up, Koroshetz says. The neurons responsible for moving that arm are gone, but in many cases new neurons will pitch in to get the fingers wiggling.
An MRI can give physicians a sense of how much damage the brain has sustained and what areas are affected, Koroshetz says, but it isn’t necessarily a good predictor of patient recovery. Age, however, does play a big role. “Young people can have amazing recoveries,” he says. “I’ve seen people with half their brains gone, and two years later you can’t tell.” Therapy also has an impact. “If you practice something in this period, it seems to improve your chance of getting better,” he says. Recovery tends to be most pronounced in the first three months after a stroke. By six months, the recovery rate has slowed. But a new study finds that stroke patients’ ability to walk can improve even six months to a year after the stroke.
Cee has been in recovery for nearly two months. Given the severity of her stroke, her progress has been impressive. But she still struggles. Cee can make small talk, but she sometimes forgets words. And coming up with lists of vegetables or flowers — items she could have rattled off before the stroke — takes time and painstaking effort. Cee can say ‘cat’ if you show her a picture of one, but if you ask her to match the word ‘cat’ with the picture, she has trouble.
Not surprisingly, Cee gets frustrated. She remembers how easy things used to be, and she longs for them to be easy again. That’s normal, Koroshetz says. “It’s terribly frustrating not to be able to do something that you used to take for granted.”
Still, small breakthroughs happen. A couple of weeks ago, Cee moved her once-limp right arm, which she nicknamed ‘Ralph.’
Cee can’t move Ralph much (the grunt at the end should be evidence of how hard she’s working). But it’s enough to give all of us hope.
Maybe Cee won’t fully recover. But then again maybe she will. Neurologists have yet to solve all the brain’s mysteries. And I’d like to believe my aunt is far from the average stroke patient. She is a fighter. And so is Ralph.
**
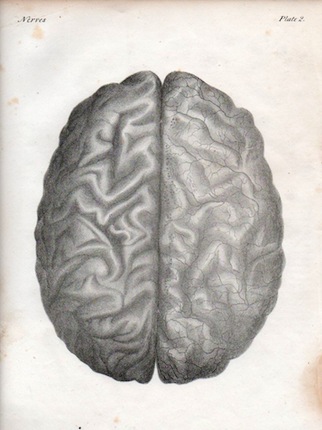
Brain lithographs courtesy of John Ptak.
More info on strokes at NINDS and the American Stroke Association.
To protect my family’s privacy, I have shortened my aunt’s name to “Cee.”
I wish your aunt the very best possible outcome. A close relative of mine suffered a series of strokes over a ten year period. Although she couldn’t really talk and was paralyzed down one side, she loved backgammon and played it well.
I would have hoped the the person from NINDs would have at least mentioned neuroplasticity and neurogenesis and talked about the recent research into stopping cell death in the penumbra and assisting recovery in the penumbra: tumeric, anti-depressants, stopping glutamate poisoning, enteracept, enhanced sti umulation, music therapy. Eveyone is completely on their own. A well-planned national initiative would be more effective instead of piecemeal as is happening now. But I don’t see any of the national stroke associations doing this since they are not for survivors. 6 million US survivors plus the thousands of doctors and therapists treating stroke survivors all looking for the same thing is a total waste of time and effort. Get a stroke survivor in charge and it will be accomplished. Jill Boltes’ recovery is not useful since there was no damage diagnosis. ie. what area was dead vs. what was partially damaged and in the bleed drainage area.
Rosie, thanks for the message.
dean r, Dr. Koroshetz did mention neuroplasticity. Wouldn’t the ability of neurons to take on new roles fall into that category? With respect to neurogenesis, growing new neurons, Koroshetz told me that brain stem cells migrate to the periphery of the damage. What they do once they arrive is still unclear. He said this might account for the age differences that we see — perhaps younger people have more of these stem cells, or more migration of them. It seems like there’s still a lot we have to learn.
Koroshetz seemed particularly excited by the idea of studying younger stroke patients to determine whether they have specific growth factors or other proteins that aid in their recovery. If they do, researchers might one day be able to make a drug that would help older patients recover just as well as younger ones.
Hi Cassandra,
It’s been a while since the post, any updates on your aunt’s progress?
Geoff,
Thanks for asking! She is doing awesome. I saw her in August and I would never have known she had had a stroke. She hasn’t made a full recovery — Ralph still gives her some trouble — but she’s well on her way.