- India
- International
A pandemic is never absolutely over, but it can be controlled: Dr Naresh Trehan
"In any country, let alone a country the size and complexity of India, not everyone and not even large sections of the population can be immunized in the short or medium term. This takes years, even decades," says Dr Naresh Trehan
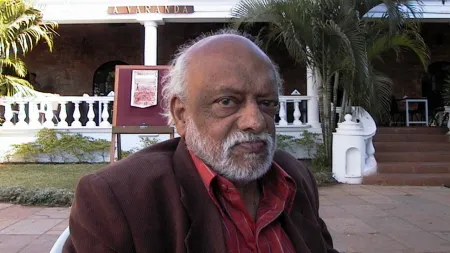
 The healthcare sector -- the importance of which was underscored by recent government initiatives -- emerged as the bulwark against this pandemic, says Dr Naresh Trehan. (Source: PR handout)
The healthcare sector -- the importance of which was underscored by recent government initiatives -- emerged as the bulwark against this pandemic, says Dr Naresh Trehan. (Source: PR handout)The raging pandemic has become a relentless part of our lives. In its effort to contain it, the world has been scrambling and scouting for answers. Doctors, nurses and other healthcare officials have been working tirelessly to help the affected and scientists and researchers have been trying to find a solution in the form of a vaccine that could end the pandemic once and for all.
But does a pandemic really end? And does the infection go away, or does it bury itself in limbo? People around the world have been asking their own questions, hoping against hope that they find their health and closure.
In an email interaction with indianexpress.com, Dr Naresh Trehan, Chairman and Managing Director of Medanta Hospital, shed light on the constant evolution of the healthcare sector, the need for governments to build more hospitals, and the time it may take to inoculate a country as vast as India, among other things.
Excerpts:
How much has the healthcare sector evolved during the pandemic?
The healthcare sector — the importance of which was underscored by recent government initiatives — emerged as the bulwark against this pandemic. This centre-stage position will only grow in importance and scale. A significant development has been the partnership for public health between the government and the healthcare sector, which has accelerated. This is a necessity given the scale and the momentum of this pandemic and others to follow, not to mention the otherwise pressing and overarching need for both the government and the healthcare sector to work together.

Another aspect of the revised dynamics is that the healthcare sector has had to gain greater agility, innovation and cross-functional expertise. Intra-sector dynamics has assumed greater immediacy and sense of cooperation. This augurs well.
ALSO READ | How do COVID-19 triggered blood clots affect the heart? A doctor answers
Why is the patient-first policy important?
A patient-first approach is a personalised one. It co-opts the patient in the treatment, focuses on the patient’s personal needs, wants, and goals so that the individual becomes central to the care and nursing process. Increasingly, besides treatment, health is about more than the care patients receive from providers. It is about living a healthier life, avoiding getting sick and learning about good ways to manage illness when it happens. Creating a culture of health and wellness supports patients in making educated, informed decisions about their care.
A healthcare system that puts patients first requires the input and participation of patients. In our estimation, we continue to expand how patients are engaged throughout the healthcare system. This is necessary and is gaining wide-scale importance because patients are more informed and empowered than previously; incorporating patients in treatment through their views, detailed feedbacks, co-creation of therapies and treatments leads to better results. This is also a cultural need today with the new age patient who wants to partner in the recovery and wellness process and not operate from a passive prism.
For instance, Medanta has been committed to patient-centricity since inception. The constant endeavour of providing world-class healthcare, best-in-class technology and unmatched medical expertise was recently acknowledged, as we were recognised as the best private hospital in India in the ‘World’s Best Hospitals 2020’ survey by Newsweek in partnership with Statista Inc. The rankings were done on the basis of the feedback shared by medical professionals and patients.
Have online/tele-consultations helped the doctors to serve patients better amid the pandemic? Is there scope for it in the future, too, when the pandemic is over?
Telemedicine, though underleveraged thus far, has always been an excellent medium. It is immediate, convenient, private, dedicated, detailed and agnostic to geography and logistics. At a time when social distancing is among the major measures to fight the virus, telemedicine has only emerged stronger; it has gained widespread popularity. The World Health Organization (WHO) is also promoting telemedicine as an alternative model for clinical services and clinical decision support. The Union Health Ministry has also approved the use of telemedicine by registered medical practitioners to treat COVID-19 patients. Telemedicine can offer a viable solution for challenges such as shortage of healthcare workers with unequal quality and access to healthcare. The other benefits include elimination of risk of transmission of the virus, saving on time and commutation, reduced waiting time and providing access in remote locations.
ALSO READ | Fever confusion: How to tell apart COVID-19 and the common flu?
After many months, do you think most hospitals are better prepared and better equipped now to deal with the cases?
On the whole, yes, the bar on hygiene and safety has been raised. Increasingly, we see stringent safety and hygiene measures — as recommended by the WHO — being instituted across the hospital campuses. Visitors wear masks and undergo mandatory thermal screening for assessment of COVID symptoms. The protocols begin from the entrance of the hospital where attendants and hospital staff are also thermal-screened for symptoms alongside patients. In the case of Medanta, the history of symptoms and travel is noted for every patient and any potential suspect is directed to a separate flu clinic in an isolated area for further evaluation.
To ensure safety within the hospital, sanitizers are available everywhere and frequent sanitization of the entire premises is undertaken at regular intervals. Physical distancing is maintained at all times within the premises. The staff wears appropriate PPEs and only one caregiver is allowed per patient to avoid overcrowding. Hospital staff is regularly trained on recognition of symptoms and triaging (decide the order of treatment) of sick patients and other measures as per the government guidelines.
Do you think it is pertinent now for governments to build more hospitals around the country?
In line with bridging the overall deficit in healthcare infrastructure, the government as well as the healthcare should create more facilities and, equally importantly, equip them with quality manpower and equipment. Collaborations and partnerships are equally important. In a first-of-its-kind initiative, Medanta partnered with other private hospitals in Gurugram to set up a designated COVID-19 hospital in May this year. The partnership involves providing doctors, health staff and equipment to cater to all COVID-19 patients, whether asymptomatic or critical.
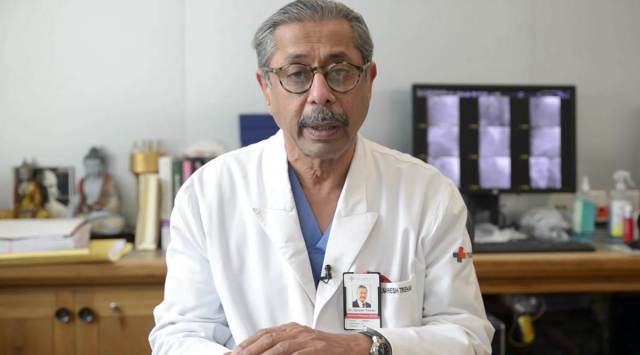
 ‘After a vaccine has been approved, it can take years to inoculate a country as big as India.’ (Source: Getty/Thinkstock)
‘After a vaccine has been approved, it can take years to inoculate a country as big as India.’ (Source: Getty/Thinkstock)
With this initiative, we also want to help non-COVID-19 patients who are waiting for their surgeries and treatments which have been/are being delayed because of the pandemic. This will also help take away the psychological fear that visiting a hospital can make people contract the virus.
ALSO READ | COVID-19 and the risk of acute pancreatitis: Here’s what an expert advises
Technically, when can we say that a pandemic is over, and how far do you think we are from that happening?
There cannot be predictions beyond a generalized rough estimate. Once the strain weakens, as the rate of spread and the rate of recovery balance out, we can consider the pandemic on a lower alarm threshold. That point has not happened yet and is some time away. At the same time it must be understood that a pandemic is never over in absolute terms. It can be controlled once the above factors come into play and once effective vaccines are discovered. Viruses remain and this one will, too. The key is containment and treatment.
After a vaccine has been approved, how much time do you think it will take to inoculate a country as vast and populated as ours?
In any country, let alone a country the size and complexity of India, not everyone and not even large sections of the population can be immunized in the short or medium term. This takes years, even decades.
How much do you think the lockdown helped in containing the spread of infection?
One lockdown, two lockdowns, no lockdowns or a smart lockdown?
It is a tenuous question and an equally tenuous answer because there are no absolutes. There’s no clear pattern, so a lockdown to prevent the increase of COVID infection must be evaluated for well-defined contexts. It is different from doing a lockdown in Wuhan than Buenos Aires or Mumbai or London. Each city has different characteristics, such as the population, economy, transport, and health systems; this changes the levels of contact that a person can have daily. It is also necessary to evaluate the lockdown for intermediate and small cities since their economic models could have damages that are almost impossible to repair.
Aside from this it’s also just very hard to imagine how a lockdown — which greatly reduces the frequency of human contact — could possibly fail to have an impact on the spread of an infectious agent. This is epidemiology in another application. Lockdowns are essential to save time and strengthen health systems that can become overloaded. The actual contagion data is limited and short, so it is necessary to prospectively evaluate each measure that public health authorities and governments wish to implement. The recommendation, according to the simulations, is to carry out an extended initial lockdown and then gradually return to activities, controlling social contacts so that at the end of this period, there should only be a maximum of 40 per cent of the contacts they had before the quarantine.
Quarantine duration times should be very cautious, as they could shift the contagion curve over time and generate a spike with a delay time.
ALSO READ | Support bubbles: What are they and should you form one?
Going forward, do you think we have a system in place now to deal with such future outbreaks?
I believe in the dictum that one can never be entirely prepared and there cannot be infallible cookie-cutter systems or approaches.
Emerging epidemics show that humans are not infallible and communities need to be prepared. Coronavirus outbreak was first reported towards the end of 2019 and has now been declared a pandemic by the WHO. Worldwide, countries are responding differently to the virus outbreak. A delay in detection and response had been recorded in China, as well as in other major countries, which led to an overburdening of the local health systems. On the other hand, some other nations have put in place effective strategies to contain the infection, and have recorded a very low number of cases since the beginning.
Restrictive measures like social distancing, lockdown, case detection, isolation, contact tracing, and quarantine of those exposed, had revealed the most efficient actions to control the disease spreading. Based on the experience of these countries, India responded to the pandemic accordingly. Only time will tell how well India has faced the outbreak. Looking into the near future, containing the COVID-19 epidemic is likely to take several months; public health interventions will be directed towards social distancing and improving hygienic practices. These interventions will be effective in delaying the onset of wide community transmission, reducing peak incidence and its impact. Testing, contact tracing, isolation of infected and precautionary self-isolation of contacts is critical in reducing the number of new cases. An exceptionally high degree of understanding in the population and acceptance of these measures is also vital.
 Restrictive measures like social distancing, lockdown, case detection, isolation, contact tracing, and quarantine of those exposed, had revealed the most efficient actions to control the disease spreading. (Source: Pixabay)
Restrictive measures like social distancing, lockdown, case detection, isolation, contact tracing, and quarantine of those exposed, had revealed the most efficient actions to control the disease spreading. (Source: Pixabay)
These interventions have to be balanced with getting back to normal life and everyday activities to the best extent possible, until a reversing the trajectory of the pandemic is tracked.
Little knowledge is available so far on alternative routes of transmission — via sewage, contaminated water, or air conditioning systems. It is also poorly known if those who have recovered from infection would be protected from reinfection. Antibody testing has to be implemented on a large scale to identify who are already immune to the virus. Multiple trials are currently underway to develop novel treatment options as well as a vaccine to treat the respiratory syndrome. Months are needed before a vaccine is developed and approved. Even though herd immunity develops over time, vulnerable groups such as the healthcare workforce and elderly people should still be preserved. Smart working and staggered shifts may have to be adopted to mitigate COVID-19 transmission in the future. Digital didactic and online learning can be protracted for months. Timely identification, efficient diagnosis, rapid isolation, and clinical management would remain key.
Over the past few months, COVID-19 has emerged as a public health threat around the world. It adds to the list of previous epidemic infectious disease outbreaks, including Bovine Spongiform Encephalitis in 1986, the avian flu in 1997, the SARS in 2002, the Swine Flu in 2009, and the Ebola in 2014. All these outbreaks remind us that we live in a habitat where it is necessary to respect the relationship between animal, social life, and the environment to survive and thrive. With COVID-19, nature is sending us a message that we need to recognize the interrelationship between animals, including pets, livestock and wildlife. The transdisciplinary one-health approach involving professionals from many disciplines such as medicine, veterinary, environmental health, and social sciences has been advocated to limit new infectious outbreaks.
For more lifestyle news, follow us: Twitter: lifestyle_ie | Facebook: IE Lifestyle | Instagram: ie_lifestyle
May 03: Latest News
- 01
- 02
- 03
- 04
- 05