Improvements in communication, personal protective equipment training, initial infection responses and social distancing have emerged as key areas of improvement if Australia is to avoid a second wave of coronavirus infections after lockdowns ease.
While the government has linked the uptake of its Covidsafe tracing app to a return to normal, the chief medical officer, Brendan Murphy, in April identified the bolstering of health authorities’ ability to respond to and contain localised clusters as an essential step to reassessing measures.
Despite Australia’s relative success in containing the virus nationwide, and the government contracting a private medical operator to help respond to declared outbreaks, the root causes behind clusters including Newmarch House, Cedar Meats abattoir, and northwestern Tasmania, have exposed key lessons in how to react to future outbreaks.
While the closure of international borders makes a repeat of the Ruby Princess debacle unlikely in the near future, leading epidemiologists are already promoting principles to stop outbreaks creating a second coronavirus wave in Australia.
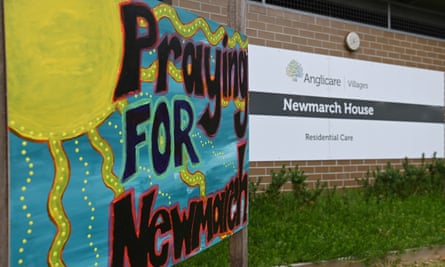
Newmarch House
Just under a month after recording its first case – a part-time carer who had worked six shifts with mild symptoms – on 11 April, the aged-care facility in Sydney’s west continues to be one of the worst Covid-19 outbreaks in the country. As of Friday, there were 69 confirmed coronavirus cases (37 residents) linked to the aged-care home, the 17th resident death was announced on Saturday.
The aged-care sector was one of the first subjected to tightened social distancing restrictions, and while a limit of two adult visitors at one time – once a day in a resident’s room was enforced nationally – many providers went further and banned physical visits to avoid the virus entering a facility.
As the sector looks set to finalise a national code for visitation to ensure all families have access to residents, the deteriorating situation at Newmarch House should change the way providers respond to initial cases, according to Joseph Ibrahim, a professor of forensic medicine and head of the health law and ageing research unit at Monash University.
While outbreaks have been seen at other aged-care facilities around the country, most notably at the Dorothy Henderson Lodge, also in Sydney, Ibrahim said residents at Newmarch should not have been allowed to remain at the home after being diagnosed.
He says this is because personal protective equipment – gloves, face masks and gowns – are difficult to wear properly for experienced hospital staff, and even harder for aged-care staff who were not properly trained in its use before the pandemic hit.
“Staff aren’t trained to do this, they shouldn’t be criticised. They’re now being asked to have a level of attention to detail regarding infection control that you would normally see in a highly specialised hospital unit, what you’d normally see with oncology patients.”
Breaches of PPE protocol have been levelled against several Newmarch staff, including against one surge staff clinician contracted by the federal government. Ibrahim said breaches are to be expected given the level of infection control required and activities involved in aged care.
“It’s not as straightforward as everyone thinks. Let’s say there’s 30 staff, and they’ve got to see a resident three times a day. That means they have to put on and take off PPE 90 times, which is 180 conditions of use. So if they follow it right 90% of the time, then there’s still 18 breaches.”
Ibrahim says it’s too late to evacuate remaining Covid-19 positive residents to stop the spread in Newmarch, but says governments should appoint aged-care facility controllers to be in charge of groups of homes, and for them to report infections and issues regarding PPE and management to the health authorities as soon as they arise.
Cedar Meats
Revelations this week that staff at the Melbourne meat processing plant now linked to 62 cases of Covid-19 were not informed they could stay away from work for several days after the company had been told two workers were infected, have highlighted shortcomings experts warn need to be addressed.

While operator Cedar Meats was informed by the Victorian Department of Health and Human Services on 27 April that a worker had tested positive the previous day, it has emerged an earlier employee case was diagnosed, but not reported to the operator at first instance, because they had been contracted by a labour hire company.
Further reports of an earlier confirmed case at the facility was recorded as early as 2 April, and an account from a worker who told the Guardian on the condition of anonymity that they were “very scared” but felt they couldn’t stay home from work after a case was announced later in April. These cases show the importance of communication protocols and employer messaging, says Peter Collignon, a professor of infectious diseases at the Australian National University.
“This is going to be a problem as businesses reopen, when you have contractors and subcontractors, and not just in abattoirs but also cleaners who work in hospitals via labour hire companies.”
Collignon thinks the “communication chain needs to be better than what’s occurred in the past”, and wants to see a protocol for notification of a confirmed case introduced so state health authorities, employers, employees and labour hire companies are all looped in.
“There just needs to be a much more transparent process once there’s that first diagnosis.”
Collignon says future clusters are “unavoidable”, but thinks what poses a greater risk of them causing second waves of Covid-19 is an attitude that workers feel they need to go into work.
He says employees need to feel comfortable they won’t risk their job safety if they don’t turn up for work and must assume any sickness or symptoms they notice could be Covid-19 and to get tested.
“Overwhelmingly you see clusters and outbreaks are occurring around working environments, because people are presenting to work when sick, often with mild symptoms.
North-west Tasmania outbreak
Collignon also says worker attitudes were the most important lesson authorities took from the outbreak of coronavirus cases at a hospital in north-west Tasmania in early April, which saw two hospitals in Burnie shut, non-essential business banned, and more than 1,000 healthcare workers and up to 4,000 family members forced into self isolation.
While an interim report into the outbreak found the initial cluster was linked to cases from the Ruby Princess, it made key recommendations including the digitisation of staff rosters to aid communication and contact tracing, the limiting of staff and patient movement between facilities, and addressing the underlying reasons behind staff working when sick.

Collignon says mildly sick workers must not feel they need to go into work to support colleagues, especially in a healthcare and aged-care setting.
“Where we’ve seen clusters, either people have gone to work when sick, in nursing homes, like at Newmarch, where they’re going to have to be closer than a metre and a half to the residents when they work. But also in the hospital in Tasmania.
“Often it’s staff who think they’re different and don’t have to stick to the rules. The reality is people went to work when they were sick and people didn’t keep physical distancing. These outbreaks were avoidable.”
Collignon also says while a workplace-wide shutdown was the default reaction before lockdowns came in, future clusters wouldn’t require an entire office or facility to close if employers enforced social distancing in their reopened offices.
“The advantage for bosses making sure the 1.5 metre distancing rule is observed, means there’s a markedly lower chance that one worker being diagnosed will require everyone to quarantine. Outbreaks can be avoided if they keep distancing.”
