THE DOMINIC COOPER BLOG
Exploring Britain’s national work-related mental health statistics
The HSE’s annual statistics on work-related ill health and workplace injuries highlighted wellbeing as a cause for concern. Dominic Cooper says further analysis is required to reveal the true picture. Here he crunches the numbers.
Everywhere we look, there is a glut of organisations telling us that most of us are stressed out, anxious or depressed from our work. Based on self-report and perceptual surveys, some state it is one of the main reasons for sickness absence1, while the Office of National Statistics (ONS)2 shows it is less of a sickness absence problem than minor illnesses, musculoskeletal problems, or other issues (accidents, poisonings, infectious diseases, skin disorders and diabetes).
According to the British Health & Safety Executive’s (HSE) annual Labour Force Survey (LFS), the main workplace stressors are workload, tight deadlines, too much responsibility, a lack of managerial support and poor relationships with co-workers. We all cope differently with such things: some thrive, most tolerate, while some can no longer function and visit their GP for stress-related diagnosis and treatment (most of the latter work in professional or technical occupations). Given the scale and scope of this ever-increasing stress crisis, curiosity got the better of me: what story is really being told by the ‘official’ national statistics over the past decade or two?
THOR-GP records of work-related MH cases
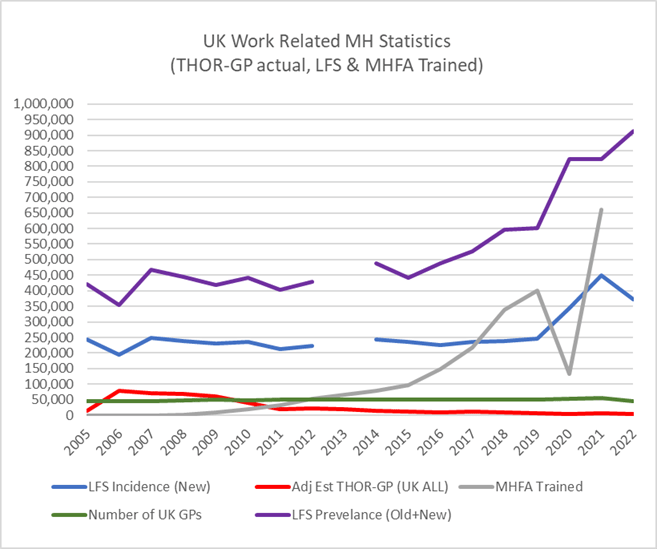
My first port of call was the Centre for Occupational and Environmental Health (COEH) at the University of Manchester (my old alma mater), which administers a general practitioners (GPs) surveillance scheme (THOR-GP) for reporting new cases of work-related ill-health across the UK. They very kindly provided me with the number of mental health (MH) cases reported to them since 2005, as well as the number of reporting GPs3. Dividing the annual number of UK GPs4,5,6 by the corresponding number of THOR reporting GPs, then multiplying the reported MH cases by the product provides a much better estimate of annual national MH totals. As shown in the Figure below, since 2005, the actual number of reported debilitating workplace stress, anxiety and depression cases has reduced significantly. Raising awareness of the issue certainly seems to have led to people seeking and receiving treatment to good effect. Hallelujah, it seems we have cracked the problem.

UK Work-Related Mental Health Statistics
HSE labour force survey data
Woah….. not so fast! This ‘success’ story changes dramatically when HSE annual LFS new case data is trended in Figure 1. The trend is relatively static, at around the 250K mark, from 2005 until 2019 where it begins to increase, reaching 450K cases by 2021 during COVID, though it has since dropped back to 372K cases in 2022. Thus, the LFS data is adding to the impression that Britain is in the grip of a massive work-related stress pandemic. When the LFS measurement process itself is explored, it’s apparent that the data is obtained from quarterly distributions that count a large proportion of the same people’s responses multiple times over a year or more, about their MH experience over the previous 12 months. Thus, the self-report LFS MH cases appear to be substantially inflated by the data collection method. The HSE splits the obtained data into two trends: new cases (incidence data), and old and new cases combined (prevalence data) using a 3-year moving average. The prevalence data trend in Figure 1 appears to show a dramatically worsening MH situation from 2014 to now, with a headline number of 914,000 cases in 2022. Given that the average number of days lost per diagnosed MH case is 30.6 days7 it is a bit surprising to discover that a 3-year rolling average is used to convey the status of the workplace MH issue to the nation. Such data suggests MH treatments are not working, which cannot be true as interventions to address PTSD (a chronic mental health condition) appear to be effective8.
Number of workers trained in Mental Health First Aid
 It was around 2014/15 that the great and the good of Britain’s workplace professions (British Safety Council, IIRSM, RoSPa, BPS, CIPD, HSE, IOD, CBI, etc.) introduced a coordinated and concerted effort to address workplace MH issues. OSH was deemed to be at the forefront, with a steady stream of publications and conferences pushing the MH agenda ever since, accompanied by a rise in Mental Health First Aid (MHFA) courses as a commonly promoted remedy. Curious about the impact of that, I visited their website, downloaded and trended the number of workers they say have been trained since MHFA came over from Australia in 2008 – shown in the figure above. The overlap between the number of MHFA-trained workers with the number of ‘new’ LFS self-report MH cases is 50% (r= 0.70, p<=0.01), and 55% with the LFS prevalence data (r= 0.74, p<=0.01), suggesting the rising number of self-report cases since 2015 is largely attributable to the marketing of workplace MH by the professions and other vested interests. In other words, it has become, or is becoming, a self-fulfilling prophecy: the more MH cases self-reported via the LFS the more MHFA training is thought to be required. The more MHFA training is provided, the bigger the self-reported MH problem becomes. The obvious question is: Where does it end?
It was around 2014/15 that the great and the good of Britain’s workplace professions (British Safety Council, IIRSM, RoSPa, BPS, CIPD, HSE, IOD, CBI, etc.) introduced a coordinated and concerted effort to address workplace MH issues. OSH was deemed to be at the forefront, with a steady stream of publications and conferences pushing the MH agenda ever since, accompanied by a rise in Mental Health First Aid (MHFA) courses as a commonly promoted remedy. Curious about the impact of that, I visited their website, downloaded and trended the number of workers they say have been trained since MHFA came over from Australia in 2008 – shown in the figure above. The overlap between the number of MHFA-trained workers with the number of ‘new’ LFS self-report MH cases is 50% (r= 0.70, p<=0.01), and 55% with the LFS prevalence data (r= 0.74, p<=0.01), suggesting the rising number of self-report cases since 2015 is largely attributable to the marketing of workplace MH by the professions and other vested interests. In other words, it has become, or is becoming, a self-fulfilling prophecy: the more MH cases self-reported via the LFS the more MHFA training is thought to be required. The more MHFA training is provided, the bigger the self-reported MH problem becomes. The obvious question is: Where does it end?
Implications
It is difficult to determine the true extent of Britain’s national workplace MH problem. Although both data sources appear to concern only lost-workday cases, THOR-GP recorded medical cases (adjusted for the entire UK) are certainly of a much lower magnitude than those suggested by the self-report LFS. Evidence9 exists that self-report survey incidents are much higher than actual clinicians’ reports. This discrepancy presents a real problem for British employers, who are being constantly urged to commit finite resources (human and financial) to tackle an MH pandemic that, in reality, is less of a problem than minor illnesses, musculoskeletal problems, or other issues (e.g., accidents). Moreover, it is acknowledged that although the ‘law’ states workplace MH must be addressed, in reality, the HSE has moved away from prosecuting such cases, as stress is a personal condition with no proven clinical methods of testing for it, and the root cause of the condition is not easily identifiable10. Britain needs to cut through the MH ‘noise’ and stop dealing with huge volumes of self-report low-level stress, simply to ensure people who really do need serious MH help are not overlooked and the necessary resources are available from their employers.
References
(1)https://www.shponline.co.uk/stress/stress-in-the-workplace/
(2)https://www.ons.gov.uk/employmentandlabourmarket/peopleinwork/labourproductivity/articles/sicknessabsenceinthelabourmarket/2021
(3)The Health and Occupation Research network (THOR), data request no: 2023-01-THOR-GP, Centre for Occupational and Environmental Health, University of Manchester.
(4)NHS Digital General Practice Workforce Statistics
(5)https://fullfact.org/health/gps-numbers-election-health-warning/
(6)https://www.statista.com/statistics/462235/general-practitioners-employment-in-the-united-kingdom-uk/
(7)Carder, M., McNamee, R., Turner, S., Hodgson, J. T., Holland, F., & Agius, R. M. (2013). Time trends in the incidence of work-related mental ill-health and musculoskeletal disorders in the UK. Occupational and environmental medicine, 70(5), 317-324.
(8)Bisson, J. I., Ehlers, A., Matthews, R., Pilling, S., Richards, D., & Turner, S. (2007). Psychological treatments for chronic post-traumatic stress disorder: Systematic review and meta-analysis. The British journal of psychiatry, 190(2), 97-104.
(9)Hussey, L., Turner, S., Thorley, K., McNamee, R., & Agius, R. (2010). Comparison of work-related ill health reporting by occupational physicians and general practitioners. Occupational Medicine, 60(4), 294-300.
(10)Bridge, S., Dilley, T., Head, C., Holmes, N., McGuinness, A., Runciman, S., Smith, R., Wiltshire, K. & Witts, R., (2013). Is stress the elephant in the boardroom? CII New Generation Programme 2013/2014.
Exploring Britain’s national work-related mental health statistics
SHP hears from Dominic Cooper, who examines work-related mental health statistics and its implications.
Dominic Cooper
SHP - Health and Safety News, Legislation, PPE, CPD and Resources Related Topics
Drug and alcohol testing in a UK airport environment
Almost half of UK manufacturing employers have increased spending on workforce health and wellbeing
‘PPE isn’t meant to be uncomfortable’: Katy Robinson and Karl Simons on inclusive PPE

 It was around 2014/15 that the great and the good of Britain’s workplace professions (British Safety Council, IIRSM, RoSPa, BPS, CIPD, HSE, IOD, CBI, etc.) introduced a coordinated and concerted effort to address workplace MH issues. OSH was deemed to be at the forefront, with a steady stream of publications and conferences pushing the MH agenda ever since, accompanied by a rise in Mental Health First Aid (MHFA) courses as a commonly promoted remedy. Curious about the impact of that, I visited their website, downloaded and trended the number of workers they say have been trained since MHFA came over from Australia in 2008 – shown in the figure above. The overlap between the number of MHFA-trained workers with the number of ‘new’ LFS self-report MH cases is 50% (r= 0.70, p<=0.01), and 55% with the LFS prevalence data (r= 0.74, p<=0.01), suggesting the rising number of self-report cases since 2015 is largely attributable to the marketing of workplace MH by the professions and other vested interests. In other words, it has become, or is becoming, a self-fulfilling prophecy: the more MH cases self-reported via the LFS the more MHFA training is thought to be required. The more MHFA training is provided, the bigger the self-reported MH problem becomes. The obvious question is: Where does it end?
It was around 2014/15 that the great and the good of Britain’s workplace professions (British Safety Council, IIRSM, RoSPa, BPS, CIPD, HSE, IOD, CBI, etc.) introduced a coordinated and concerted effort to address workplace MH issues. OSH was deemed to be at the forefront, with a steady stream of publications and conferences pushing the MH agenda ever since, accompanied by a rise in Mental Health First Aid (MHFA) courses as a commonly promoted remedy. Curious about the impact of that, I visited their website, downloaded and trended the number of workers they say have been trained since MHFA came over from Australia in 2008 – shown in the figure above. The overlap between the number of MHFA-trained workers with the number of ‘new’ LFS self-report MH cases is 50% (r= 0.70, p<=0.01), and 55% with the LFS prevalence data (r= 0.74, p<=0.01), suggesting the rising number of self-report cases since 2015 is largely attributable to the marketing of workplace MH by the professions and other vested interests. In other words, it has become, or is becoming, a self-fulfilling prophecy: the more MH cases self-reported via the LFS the more MHFA training is thought to be required. The more MHFA training is provided, the bigger the self-reported MH problem becomes. The obvious question is: Where does it end?
‘Britain needs to cut through the MH ‘noise’ and stop dealing with huge volumes of self-report low-level stress, simply to ensure people who really do need serious MH help are not overlooked and the necessary resources are available from their employers.’ This does rather sound like ‘stop whinging and pull yourselves together’. The reality is that work related stress and burnout is a major issue for employers and it is costing the UK economy an awful lot of money.
Work-related stress / burnout being a major issue for the UK economy is one of the motivators for exploring the data. Given there are 32.8 million UK businesses / entities, the LFS new data shows 0.0007 average cases per entity, while combined 3 year average data shows 0.008 avg cases per entity. In terms of sickness absence it lags behind minor illness, MSD and accidents, diabetes, skin disease etc. Thus the actual data does not seem to support the assertion. We need to hear from Business / Organisations to find out the true extent of the ‘butchers bill’ so to… Read more »
The Self-Reported part of the LFS data does show that Stress / burnout does account for more than half of the total, almost double that of MSDs. This does ring true with what I am seeing in my sector. As you say, that may be in part to how the information is collected. I would be wary of NHS data as few cases I have seen ‘up close’ have actually been anywhere near the NHS as the mental health services are typically so poor – there is little point in doing so.
Dominic’s point of that statement was “…to ensure people who really do need serious MH help are not overlooked and the necessary resources are available from their employers.”
Until we change the law to align illness and injury, we will I fear continue to see so much underreporting in this area…once upon a time people who had to take time off work because of being injured by work were ignored… just under 30 years ago the law changed that to make companies accountable…I have said for many years, I see a future where anyone off work as a result of ‘Work Induced Illness’ physical or psychological, is notifiable to the Regulator as ‘Work Induced Injury’ is today – so Government and HSE sees the true picture as organisations… Read more »
That would be good if it happened!
Great article, Dominic.
We don’t need to debate such as the Carol Black report that suggested many if not most days lost to bad backs are actually lost to ‘stress’ because it’s like the climate change debate Dom … even if it is overstated then all the things we should be doing pro-actively to address it can only be a good thing. (Like applying Warr’s vitamin model of ‘good work’ which minimises the stress hit whilst also boosting empowerment and engagement … which means more switched on and focued workers … which is a win win all around).
Dom, you have been out of the UK too long! The “sick note” has gone for most absences and sometimes it is more about getting a note from your doctor when you go back to work not to stay off. It is that difficult for people to get an appointment with their GP in most parts of the UK that much of the absence caused by stress will never reach the NHS, let alone be statistically analysed by the NHS, whilst as has been pointed out access to mental health services in the NHS is critically lacking. Hence, at present… Read more »
I have found a number of staff not wanting to see a Doctor or go to the NHS as they feel let down by long waiting times and not being heard by the person trying to help. I know from personal experience how hard it can be to find the right person to listen and guide you in what can be a challenging time for employers and employees.