Could Better Syringes Reduce HIV Transmission?
The designers of a low-dead-space syringe hope that their innovation could hamper the disease's spread among the estimated 15.9 million people who inject drugs worldwide.
Around the world, some 15.9 million people use drugs that they inject with a needle. Though in some places HIV rates among drug users are quite low, in many Eastern European and Asian cities more than 70 percent of such drugs users have been infected with the virus. Needle and syringe exchanges can help, but according to a new paper in the International Journal of Drug Policy, another option should be investigated: Distributing so-called "low-dead-space syringes," which in laboratory settings have been show to dramatically reduce the likelihood of HIV transmission.
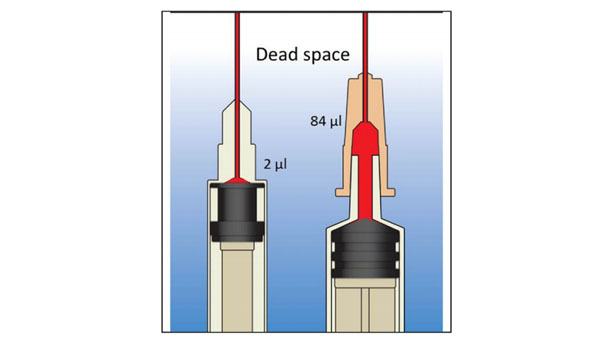
Dead space is the part of the syringe where fluid is retained once the plunger is fully depressed. High-dead-space syringes retain fluid both in the syringe itself and in the needle; low-dead-space syringes expel all the fluid in the syringe, retaining only a small amount of fluid. (In low-dead-space syringes, the needle is not detachable.)
In experiments that mimicked drug injections, the high-dead-space syringes retained 1,000 times as many microliters of blood, even after rinsing. For people carrying HIV with viral loads between one million copies and 2,000 copies per milliliter, the capacious syringes could carry multiple copies of HIV, "whereas," William A. Zule and his coauthors write, "low-dead-space syringes would retain even a single copy only a fraction of the time."
There are many hurdles to reducing HIV transmission with this strategy: How will manufacturers get the new needles to drug users? What percent of users need to use these syringes what percent of the time for the intervention to have an effect? Will people be turned off by the syringes' small size and the non-detachable needles? Would the lower-risk syringes provoke any changes in behavior that negate their benefits? But the authors contend that the potential decline in HIV transmission among drug users is substantial. For example, they estimate that China could see something like this if drug users switched over to the new syringes at a rate of 20 percent per year starting this year (an optimistic projection):
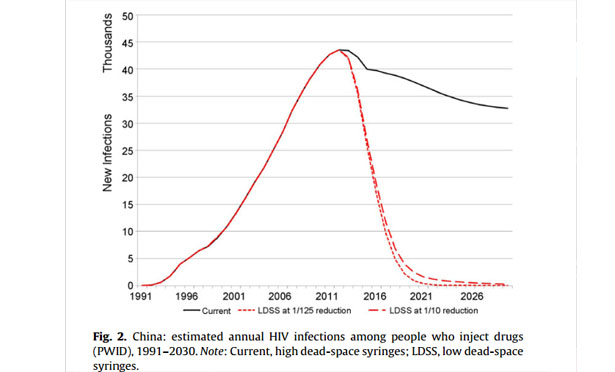
In an 18-year-period, the total number of injections spared could top 500,000, the authors claim, a reduction that would have spillover effects into the greater population at large, as those uninfected people would not transmit the disease to non-drug-users as well.
The authors argue that programs to distribute the low-dead-space syringes should be implemented quickly -- particularly in places with high rates of HIV among drug users -- and studied carefully as they roll out. Such programs certainly won't displace other HIV reduction and treatment measures, but they could supplement them powerfully.
